Revision Rhinoplasty in Melbourne
Revision rhinoplasty, also known as secondary rhinoplasty, is performed after previous nose surgery to address concerns involving nasal shape, structure, or function. If you’re considering revision rhinoplasty in Melbourne, a consultation can clarify contributing factors and assess whether these issues may be addressed, including key limitations and risk–benefit considerations.
When Revision Rhinoplasty May Be Considered
Revision rhinoplasty, also referred to as secondary rhinoplasty, is performed to address functional or aesthetic concerns following a previous nose surgery. Unlike primary procedures, revision surgery involves operating on tissue that has already healed, sometimes with scarring or altered anatomy.
These procedures require careful assessment of nasal structure, airway function, and tissue quality to determine what refinements may be achievable. While some minor revisions can be straightforward, others may be more complex due to reduced cartilage availability or previous structural changes.
For this reason, patients are encouraged to seek consultation with a surgeon who holds specialist registration (FRACS) and has specific experience in secondary nasal surgery.

Learn more about Dr Rodrigo Teixeira and his approach to plastic surgery and patient care.
Common Reasons for Revision Rhinoplasty
People seek revision rhinoplasty for different reasons. Common concerns after a primary procedure include:
- asymmetry or contour irregularities
- nasal obstruction or airflow limitation
- internal or external valve narrowing affecting airflow
- reshaping that did not settle as planned
- loss of structural support affecting function or stability
These concerns range from minor issues, where risks may outweigh potential benefit, to changes that affect function or overall facial balance. Each case requires individual assessment to determine whether revision rhinoplasty is appropriate, with consultation focused on weighing risks, benefits, and the likelihood of meaningful improvement.
The Revision Rhinoplasty Procedure (Techniques & Steps)
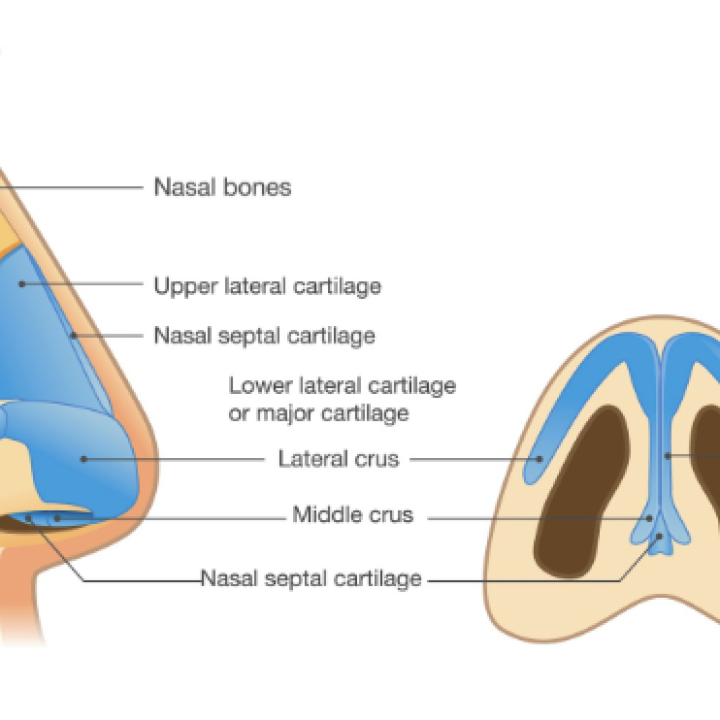
Revision rhinoplasty generally follows reconstructive principles rather than simple reshaping. The exact steps depend on the findings during examination and intra-operative assessment of the changes created by the initial surgery. Techniques commonly used in revision surgery may include:
- Open approach rhinoplasty, allowing precise access to altered structures and facilitating both functional and aesthetic refinement.
- Cartilage grafting (septal, ear, or rib) to restore support, improve projection, reinforce weak areas, or refine contour.
- Targeted structural reshaping of the bridge, sidewalls, or tip to address asymmetry, improve definition, or restore balance.
- Correction of nasal valve or airflow issues, supporting functional improvement where obstruction is present.
- Management of scar tissue or adhesions and adjustments for skin thickness, recognising that thin skin may reveal small irregularities while thick skin may limit definition.
Each technique is selected to support nasal function, stability, and balanced shape, acknowledging that outcomes vary depending on tissue quality, scarring, healing patterns, and prior surgical alterations.
Dr Rodrigo Teixeira’s Approach to Revision Rhinoplasty
Dr Teixeira’s approach prioritises openness and shared understanding. Revision surgery is only offered when he believes it is in the patient’s best interests.
Key considerations include:
- Motivation and concerns – understanding why revision is sought and whether the concerns are surgically addressable.
- Psychological readiness – discussing expectations, resilience, trust, and whether a psychological assessment may be appropriate.
- Timing and healing – ensuring tissues have healed sufficiently and assessing how further maturation may influence the outcome.
- Clinical assessment – evaluating nasal structure, airway function, cartilage availability, previous changes, and individual healing factors.
- Surgical planning and decision‑making – outlining realistic options, limitations, and risks to support informed and balanced decisions.
This structured process supports informed consent, collaborative planning, and shared decision-making, with patient wellbeing as the highest priority.
What to Expect at Your Consultation
Your consultation is a detailed process designed to assess both the current condition of your nose and the outcomes of your previous surgery. This may include:
- Reviewing past surgical records and operative notes
- Physical examination of internal and external nasal structures, including functional assessment of the nasal airways
- Photographs or digital imaging to support communication and planning
- Discussing your goals and understanding what is realistically achievable
- Considering whether a psychological assessment may be appropriate to support readiness and expectations
This conversation provides clarity about the anticipated course of treatment, possible limitations, and the expected recovery timeline.

Risks & Challenges of Revision Rhinoplasty
Revision rhinoplasty carries unique challenges compared to primary surgery and carries risks. In revision rhinoplasty, these risks may be influenced by individual healing responses and changes from earlier procedures. General surgical risks may include bleeding, haematoma, infection, anaesthetic complications, delayed wound healing, and scarring. Procedure specific risks may include:
- asymmetry, irregularities, lumps and bumps
- reshaping or correction that does not settle as planned
- graft movement, absorption, or warping
- persistent or new breathing difficulties
- unpredictable healing with prolonged or uneven swelling
Understanding these risks, and how individual factors may influence them, supports balanced and informed decision-making.
Recovery & Aftercare
Recovery varies between individuals and may take longer than after primary rhinoplasty, especially when grafting or structural reconstruction is required.
Early recovery (first week): swelling, bruising, congestion, and pressure are common. You may be advised to keep your head elevated, avoid nose blowing, protect the nose from accidental impact, and keep dressings or splints in place as instructed.
Weeks 2–6: swelling gradually settles, and many people feel ready to return to work or light activities. Strenuous exercise and activities that risk nasal injury are usually avoided.
Months 3–12: subtle swelling continues to improve, and shape refinement progresses. The final outcome may take 12 months or longer to stabilise, especially in the nasal tip.
Regular follow‑up appointments allow progress to be monitored and support provided throughout recovery.
Our Melbourne Clinic & Facilities
Consultations, assessments, and post-operative reviews take place at our Ivanhoe East rooms, a professional and private setting designed for detailed examination, imaging, and discussion of your goals, while all revision rhinoplasty procedures are performed in accredited Melbourne hospitals supported by a qualified surgical and anaesthetic team to ensure safety throughout the peri-operative period.
FAQs
Revision rhinoplasty is surgery performed after a previous rhinoplasty to address structural, functional, or aesthetic concerns that were not resolved or developed during healing.
Revision procedures can be more involved than primary rhinoplasty and may require additional operative time or grafting, which can influence total cost. A personalised estimate is provided after consultation.
Revision rhinoplasty is a recognised part of nasal surgery practice. People may seek revision for functional issues, changes in appearance after healing, or concerns that have arisen over time.
All surgery carries risks. Revision rhinoplasty may involve added considerations due to changes from previous surgery, but when performed by a qualified surgeon in an accredited facility, risks are managed using established surgical and safety principles.
Primary rhinoplasty is performed on untouched anatomy. Revision rhinoplasty involves previously operated tissue, which may include scar tissue, altered support, or limited cartilage availability, influencing planning and technique.